Oxidative Stress Associated with Poor Sleep Undermines Health, Mental, and Physical Performance, NanoVi helps Address it
We all know the importance of a good night’s sleep, especially when it eludes us. Yet quality sleep is something that a staggering number of people struggle to get. At least 50 million Americans are known to suffer from some type of sleep disorder1, and similar statistics from around the world demonstrate this disturbing reality is truly global2–4. When we think of inadequate sleep, we often recall tiredness, sluggishness, and reduced mental and physical performance. These obvious symptoms, however, exist in addition to—and may in fact stem from—the impact that poor sleep has within our cells.
Poor Sleep Causes Oxidative Stress Damage
One of the most profound and concerning cellular changes caused by insufficient sleep is the induction of oxidative stress. This phenomenon leads to oxidative damage, which occurs when the formation of molecules known as reactive oxygen species (ROS) overwhelms our cells’ ability to neutralize and detoxify them, leading to molecular damage5. This damage involves ROS attacking important parts of the cell, from lipids—which are the building blocks of the cell membrane—to proteins and DNA6–9.
The relationship between lack of sleep and oxidative stress is well researched. Quite simply, sleep deprivation promotes a state of oxidative stress in living tissues10. This damage occurs—among other places—in vital organs like the liver and heart11,12, and oxidative balance is restored by rest and sleep11. Sleep and oxidative stress are so closely joined at the hip that some research suggests an increase in ROS in the part of the brain that regulates sleep may, in fact, help to induce sleepiness13—likely as a way of promoting the rest and recovery our bodies need when facing oxidative stress.
Sleep Disorders Cause Additional Oxidative Stress Damage
Unfortunately for the many individuals who suffer from one particular sleep disorder, strong evidence links obstructive sleep apnea to its own specific risk of increased oxidative stress induction14–21. Rather than sleep deprivation alone, the reason for this increase in oxidative damage is believed to result from intermittent hypoxia (low oxygen delivery) resulting from airway obstruction during sleep14,16,17. This correlation is explained by the way that ROS are formed.
Oxygen Levels Matter – Ideally Not too High or too Low
As might be surmised from their name, reactive oxygen species are created through chemical reactions involving oxygen, often when cells use oxygen to make energy through a process called aerobic metabolism9. Unsurprisingly, high oxygen concentration (or hyperoxia) is known to increase ROS formation and oxidative stress22–24. Somewhat confusingly, ROS formation and the resulting cell damage can also come from too little oxygen (or hypoxia) in our cells as well25. The trick for the body, then, is to balance oxygen levels at a healthy middle ground—something that does not happen consistently enough in obstructive sleep apnea.
Why Improving Protein Functions Helps
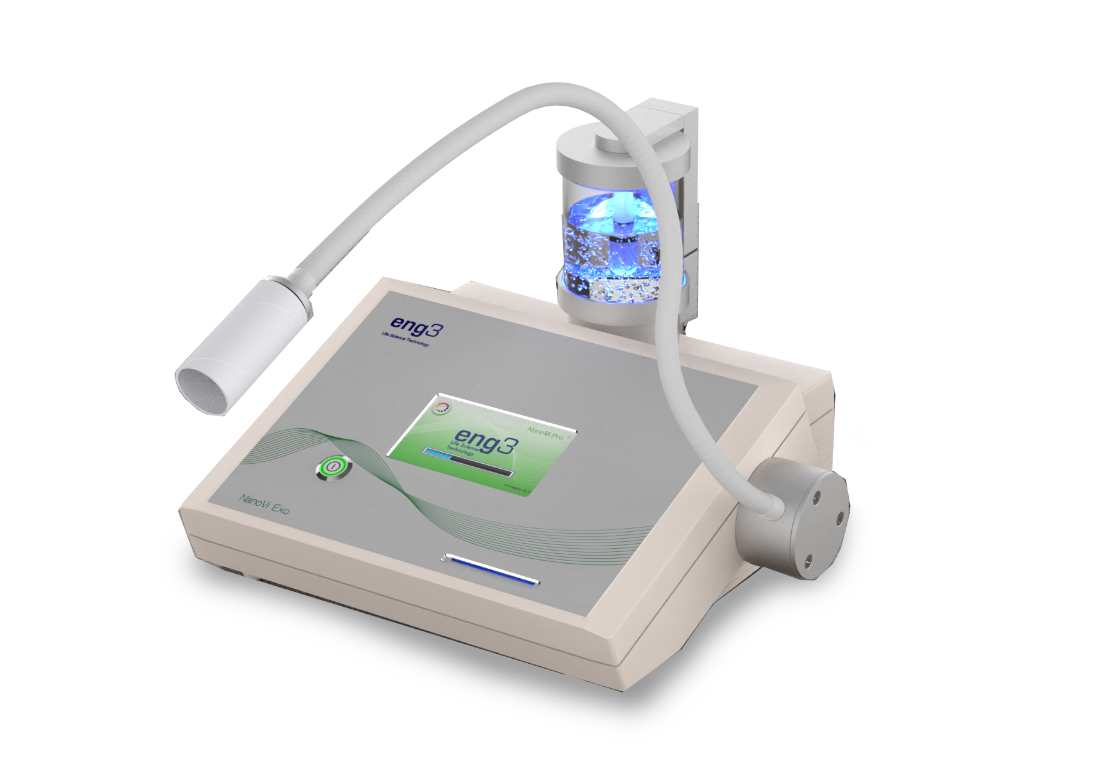
Eng3’s NanoVi® device is designed to help combat the oxidative stress and cell damage that so often occurs as a result of sleep disorders. By eliciting the increased creation of ordered water within cells, NanoVi upregulates the efficiency of protein folding. Since proteins are extremely important in deciding how our cells operate, and since the folded shape of a protein is imperative to determining its function, improving the reliability of correct protein folding increases the wellness of our cells and, ultimately, the whole body.
Improved protein function directly impacts the cell’s ability to fight the negative effects of oxidative stress. As previously addressed, ROS damage our cells by attacking vital cell components. When proteins are attacked and oxidized, they can unfold and lose their ability to function properly. Many proteins are directly responsible for combating oxidative stress, including proteins that detoxify ROS, assist fellow proteins to refold, or repair damage to DNA8,26. If these proteins are harmed by ROS, cellular damage can spiral out of control unless the proteins are able to recover quickly.
Counteract the Oxidative Damage of Poor Sleep
The NanoVi device helps proteins recover from damage quickly. Robust scientific research highlights how NanoVi improves resistance to oxidative stress and cellular health. A recent report demonstrates how proteins treated with NanoVi are able to recover from oxidative damage much faster than proteins without NanoVi treatment27. Moreover, the same research showed that individuals treated with NanoVi produce higher levels of several key antioxidant proteins known to fight ROS in humans. Such important findings strongly suggest that NanoVi could be an optimal way to combat oxidative stress stemming from poor sleep or any other source.
For those suffering from a chronic sleep disorder, every advantage in promoting cell health and recovery is meaningful. By helping the body’s natural defences to fight back against oxidative stress and optimize cellular efficiency, NanoVi serves as a powerful tool for reclaiming lost ground and productivity that results from sleep disorders. Through reducing the oxidative burden of inadequate sleep, NanoVi works to boost both mental and physical performance with a non-invasive and accessible technology backed by research and proven results.
If you’d like to learn more about the NanoVi device, its proven benefits, and the price, sign in below.
Eng3 will send you an email as soon as you submit the form, please check your spam filter if you don’t receive it. We only send study results and other valuable information. Your email will not be shared or flooded with promotional content.
Please check your spam filter if you do not receive our email right away.
References
1. Committee on Sleep Medicine and Research-Board on Health Sciences Policy-Institute of Medicine of the National Academies. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. (2006).
2. Stranges, S., Tigbe, W., Gómez-Olivé, F. X., Thorogood, M. & Kandala, N.-B. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 35, 1173–1181 (2012).
3. Sleep Health Foundation. Asleep on the job: Costs of inadequate sleep in Australia. (2017).
4. van de Straat, V. & Bracke, P. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int. J. Public Health 60, 643–650 (2015).
5. Pizzino, G. et al. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 8416763 (2017).
6. Phaniendra, A., Jestadi, D. B. & Periyasamy, L. Free radicals: properties, sources, targets, and their implication in various diseases. Indian J. Clin. Biochem. 30, 11–26 (2015).
7. Lobo, V., Patil, A., Phatak, A. & Chandra, N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn. Rev. 4, 118–126 (2010).
8. Kryston, T. B., Georgiev, A. B., Pissis, P. & Georgakilas, A. G. Role of oxidative stress and DNA damage in human carcinogenesis. Mutat. Res. Mol. Mech. Mutagen. 711, 193–201 (2011).
9. Schieber, M. & Chandel, N. S. ROS function in redox signaling and oxidative stress. Curr. Biol. 24, R453–R462 (2014).
10. Villafuerte, G. et al. Sleep Deprivation and Oxidative Stress in Animal Models: A Systematic Review. Oxid. Med. Cell. Longev. 2015, 15 (2015).
11. Everson, C., Laatsch, C. & Hogg, N. Antioxidant defense responses to sleep loss and sleep recovery. Am. J. Physiol. Regul. Integr. Comp. Physiol. 288, R374-83 (2005).
12. Chang, H.-M. et al. Sleep deprivation predisposes liver to oxidative stress and phospholipid damage: a quantitative molecular imaging study. J. Anat. 212, 295–305 (2008).
13. Ikeda, M. et al. Brain oxidation is an initial process in sleep induction. Neuroscience 130, 1029–1040 (2005).
14. Eisele, H.-J., Markart, P. & Schulz, R. Obstructive Sleep Apnea, Oxidative Stress, and Cardiovascular Disease: Evidence from Human Studies. Oxid. Med. Cell. Longev. 2015, 608438 (2015).
15. Carpagnano, G. E. et al. Increased 8-Isoprostane and Interleukin-6 in Breath Condensate of Obstructive Sleep Apnea Patients. Chest 122, 1162–1167 (2002).
16. Suzuki, Y. J., Jain, V., Park, A.-M. & Day, R. M. Oxidative stress and oxidant signaling in obstructive sleep apnea and associated cardiovascular diseases. Free Radic. Biol. Med. 40, 1683–1692 (2006).
17. Lavie, L. Obstructive sleep apnoea syndrome – an oxidative stress disorder. Sleep Med. Rev. 7, 35–51 (2003).
18. Lavie, L. Oxidative Stress—A Unifying Paradigm in Obstructive Sleep Apnea and Comorbidities. Prog. Cardiovasc. Dis. 51, 303–312 (2009).
19. Carpagnano, G. E. et al. 8-Isoprostane, a Marker of Oxidative Stress, Is Increased in Exhaled Breath Condensate of Patients With Obstructive Sleep Apnea After Night and Is Reduced by Continuous Positive Airway Pressure Therapy. Chest 124, 1386–1392 (2003).
20. Montesi, S. B., Bajwa, E. K. & Malhotra, A. Biomarkers of sleep apnea. Chest 142, 239–245 (2012).
21. Ntalapascha, M. et al. Oxidative stress in patients with obstructive sleep apnea syndrome. Sleep Breath. 17, 549–555 (2013).
22. Alttas, O. & Haffor, A.-S. Effects of hyperoxia periodic training on free radicals production, biological antioxidants potential and lactate dehydrogenase activity in the lungs of rats, Rattus norvigicus. Saudi J. Biol. Sci. 17, 65–71 (2010).
23. Sanders, S. P. et al. Hyperoxic sheep pulmonary microvascular endothelial cells generate free radicals via mitochondrial electron transport. J. Clin. Invest. 91, 46–52 (1993).
24. Lushchak, V. I. et al. Hyperoxia results in transient oxidative stress and an adaptive response by antioxidant enzymes in goldfish tissues. Int. J. Biochem. Cell Biol. 37, 1670–1680 (2005).
25. Debevec, T., Millet, G. P. & Pialoux, V. Hypoxia-Induced Oxidative Stress Modulation with Physical Activity. Front. Physiol. 8, 84 (2017).
26. Reichmann, D., Voth, W. & Jakob, U. Maintaining a Healthy Proteome during Oxidative Stress. Mol. Cell 69, 203–213 (2018).
rev01